Monkeypox Outbreaks Stir Fear of a New Pandemic. How Worried Should We Be?
July 13, 2022
- Author
- Jay Pfeifer
As the COVID-19 pandemic appears to recede, another virus is beginning to spread around the globe. The World Health Organization recently announced that more than 6,000 cases of a new variant of monkeypox virus have been reported in 58 countries, with most new cases centered in Europe. The virus is endemic in Africa and causes lesions and flu-like symptoms.
Even though monkeypox is far less severe than COVID-19—the fatality rate is somewhere around one percent—the long shadow of the coronavirus pandemic makes any outbreak alarming.
Davidson Biology Professor Dave Wessner focuses his research on viruses and has studied coronaviruses closely. He shares insight on the differences in the two viruses—and the public health impacts of monkeypox.
How does the monkeypox virus differ from the virus that causes COVID-19?
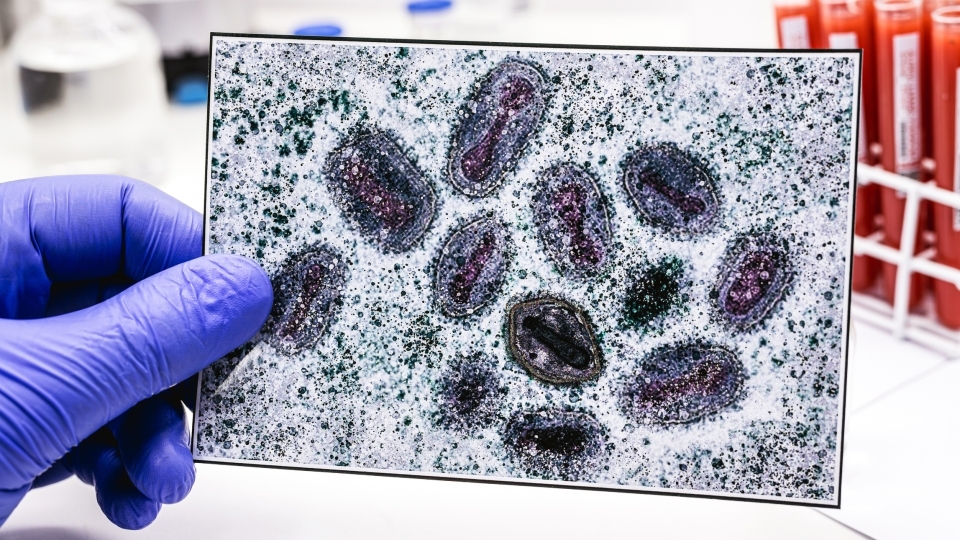
Monkeypox virus is closely related to smallpox virus, the human pathogen that was eradicated in the late 1900s. Viruses in this family are large and brick-shaped, with a length of over 300 nm and width of about 250 nm. In contrast, coronaviruses are spherical, with a diameter of about 100 nm. (To put that in perspective, a human hair is between 50,000 and 100,000 nanometers wide.) Their genomes are big, too. Poxvirus genomes are roughly 200,000 nucleotides long, whereas coronavirus genomes are about 30,000 nucleotides long.
Although monkeypox virus was first isolated from laboratory monkeys in the 1950s, monkeys are not the virus’s primary host. Like humans, monkeys probably get infected via spillover events following contact with the natural hosts. We think that various rodents probably serve as the natural hosts, but the exact species have not been determined. Historically, human-to-human transmission has been really inefficient. As a result, these occasional spillover events have resulted in only minor outbreaks. Currently, it appears that a variant of monkeypox virus has evolved that is better equipped to spread from human to human. That’s why we’re seeing this increased prevalence in areas like Europe and the United States.
Recent research shows that the virus has mutated surprisingly quickly. Is the rapid mutation a reason for elevated concern?
That evolution is the result of mutations that have occurred in the monkeypox virus genome. We’ve seen a lot of headlines recently about the large number of mutations that scientists have observed in this virus. Let’s put that in context. Researchers from the University of Edinburgh reported that the 2022 variant of monkeypox virus currently infecting humans differs from a 2018 variant of the virus at 47 sites. That’s 47 mutations within a 200,000 nucleotide genome over the past four years. In contrast, the Omicron variant of SARS-CoV-2 differs from earlier variants of this virus by about 30 nucleotides in the spike protein gene alone.
Yes, the number of mutations observed in this version of monkeypox virus is unusual, and these mutations most likely help the virus spread from person to person more efficiently. But the absolute rate of mutations is much lower than we are observing in SARS-CoV-2.
We already have a vaccine that is effective at preventing symptoms from monkeypox. How great of an advantage is that in controlling the spread of the virus?
We do have a vaccine in place, and it’s a pretty good one. Moreover, the vaccine can be administered shortly after exposure and still be effective. Plus, the transmission of monkeypox virus differs significantly from the transmission of SARS-CoV-2, which means that a very different vaccination approach could be effective.
Because SARS-CoV-2 is spread very easily and a majority of people who get infected are asymptomatic, as many people as possible need to be vaccinated to protect vulnerable members of the community. In contrast, monkeypox virus is spread only through very close, usually physical, contact. Even with transmission via respiratory droplets, it appears that the individuals must be very close together. Also, it seems that transmission only occurs once symptoms appear. Asymptomatic spread doesn’t seem to be a major factor.
So, what does this information tell us about vaccination strategies? Many infectious disease experts are recommending a ring vaccination approach. Rather than trying to vaccinate everyone, vaccinations are offered to the close contacts of every suspected case. That approach could disrupt the chain of transmission.
Are there any steps someone who hasn’t had any direct exposure to the virus should take to stay safe?
For most people, the current risk of exposure is low. But there are some precautions that are worth noting. If you have symptoms consistent with monkeypox, especially a rash on the genitals, see your healthcare provider. Identifying infected people, having them isolate and vaccinating their direct contacts is vitally important. Pre-exposure vaccinations are recommended for certain healthcare workers and clinicians who may have increased risks of exposure. People who have been in direct contact with someone with monkeypox should get vaccinated. In some places, like New York, the vaccine is being offered to people who may be at increased risk of exposure, like men who have sex with men. In addition to getting vaccinated, people should avoid direct contact with someone who has monkeypox or may have monkeypox. Of course, washing your hands frequently is a good idea!
How worried should we be?
Community spread of monkeypox virus is occurring. The virus may be mutating to become more efficient in person-to-person spread. Although the case-to-fatality rate isn’t high, the disease can be severe. So, this is a public health concern. But the risk to most people remains low. We still should be much more concerned about COVID-19.



